Collection: Best Sellers
-
G-NiiB Immunity+ Formula SIM01 | For Immune System
Regular price HK$499.00Regular price -
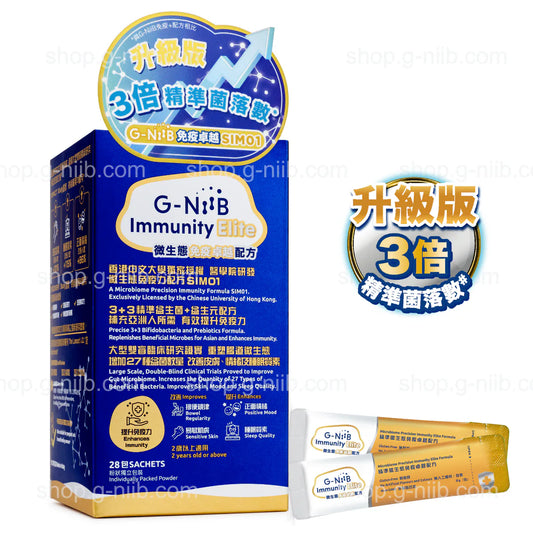
G-NiiB Immunity Elite Formula SIM01 | For Immune System
Regular price HK$568.00Regular price -
G-NiiB M3 Formula SMT04 | Gut Health Supplements
Regular price HK$549.00Regular price -
G-NiiB Skin Formula SIM05 | Skin Probiotics for Allergies
Regular price HK$559.00Regular price -
G-NiiB Liver Goal Formula SLD07 | Probiotics for Liver Fat
Regular price HK$579.00Regular price -
G-NiiB Immune Kids Formula SIM03 | Probiotics for Kids
Regular price HK$429.00Regular price -
G-NiiB Happy Child Formula SCM06 | Probiotics for Kids' Mood
Regular price HK$459.00Regular price