Early detection and removal of precancerous polyps (adenomas) can prevent CRC and reduce mortality5
The microbiome is closely related to CRC. Intestines that are persistently exposed to a hostile microbial environment have higher risks for CRC. Scientists from the Faculty of Medicine of A Renowned University in Hong Kong are among the first in the world to identify a series of bad bacteria that are specific to CRC populations. By measuring the levels of these bacteria, we detect CRC and colorectal polyps, including small polyps, and recurrent adenoma, at extremely high sensitivity. Through this measurement, we can also compute your gut microbial health, informing dietary adjustments and microbiota modulation to reduce the risk for having CRC.
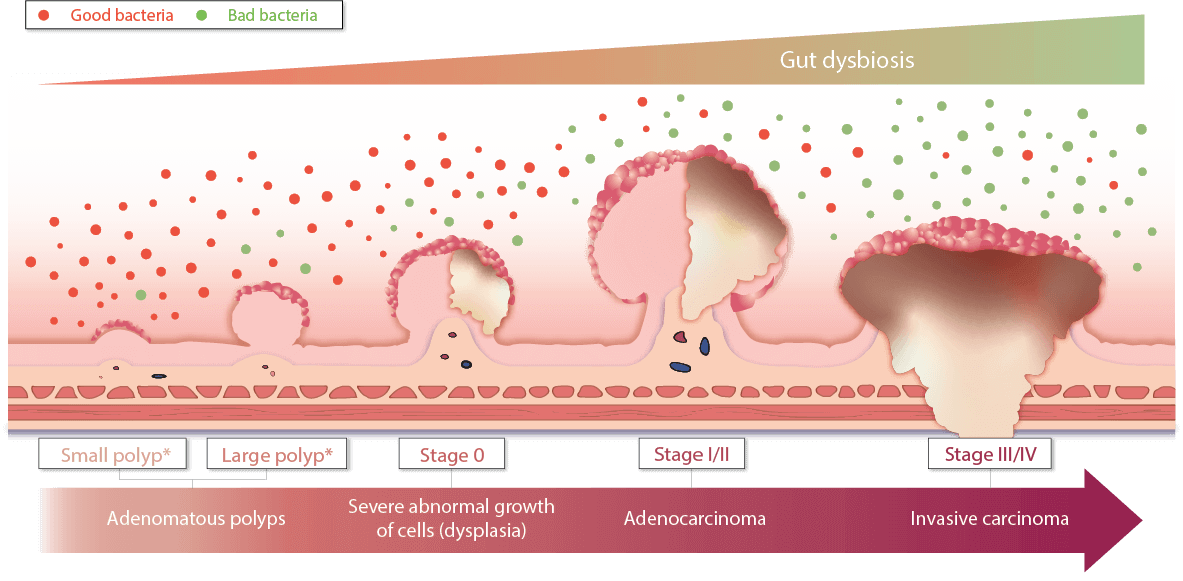
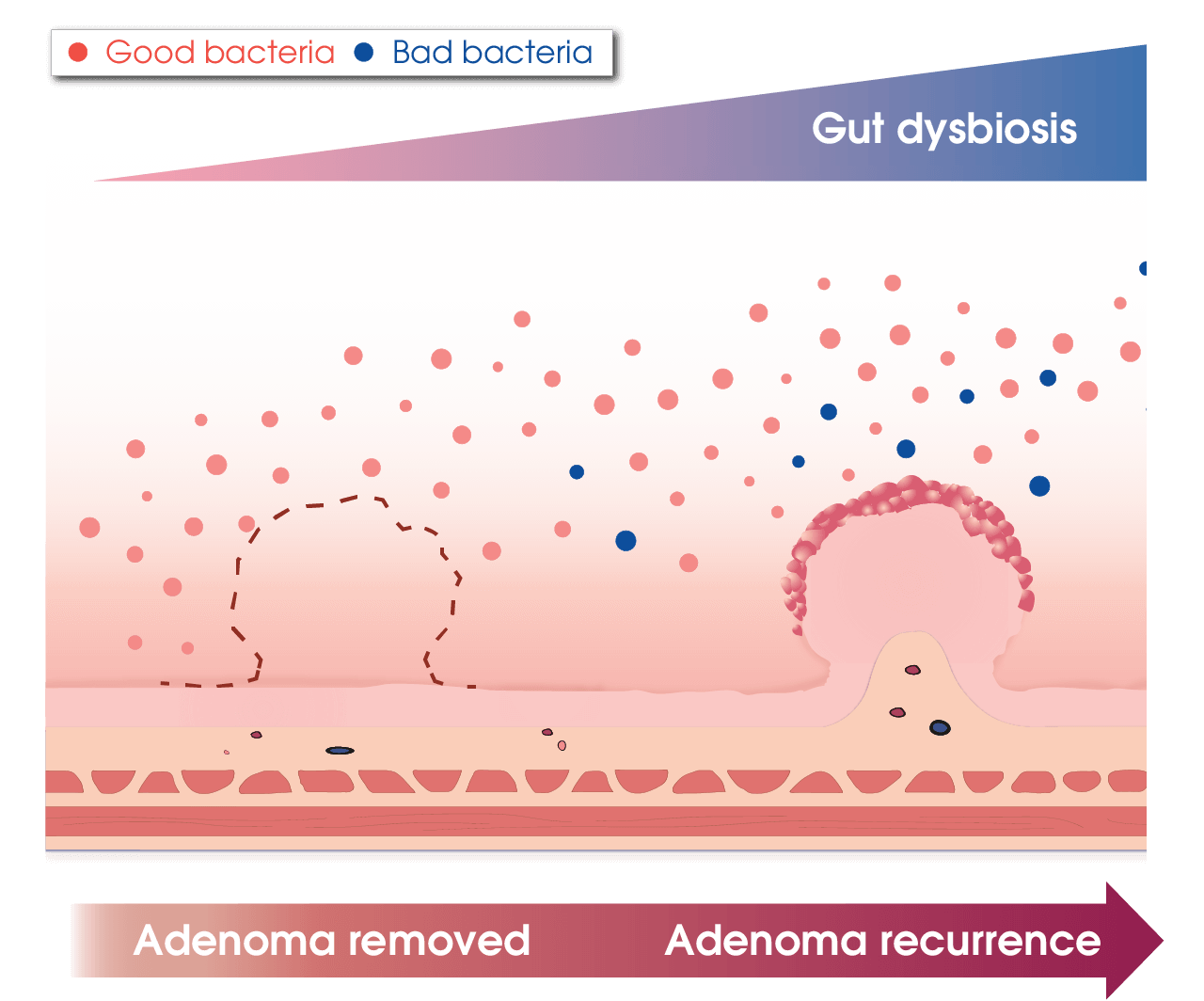
Gut Microbiome is Linked to the Development of Colorectal Cancer
We cannot edit our human genome, but we can modulate our gut microbiome to improve health
The gut microbiome dictates human health. In fact, 90% of cell counts in a human body belong to microbes, most of which reside in the intestine and interact with human cells. Studies found that:

Only 12-35% of CRC can be explained by hereditary factor6

The gut microbiome of CRC patients is different from that of healthy individuals7

Gut microbiome dysbiosis may promote cancer formation in the colon8
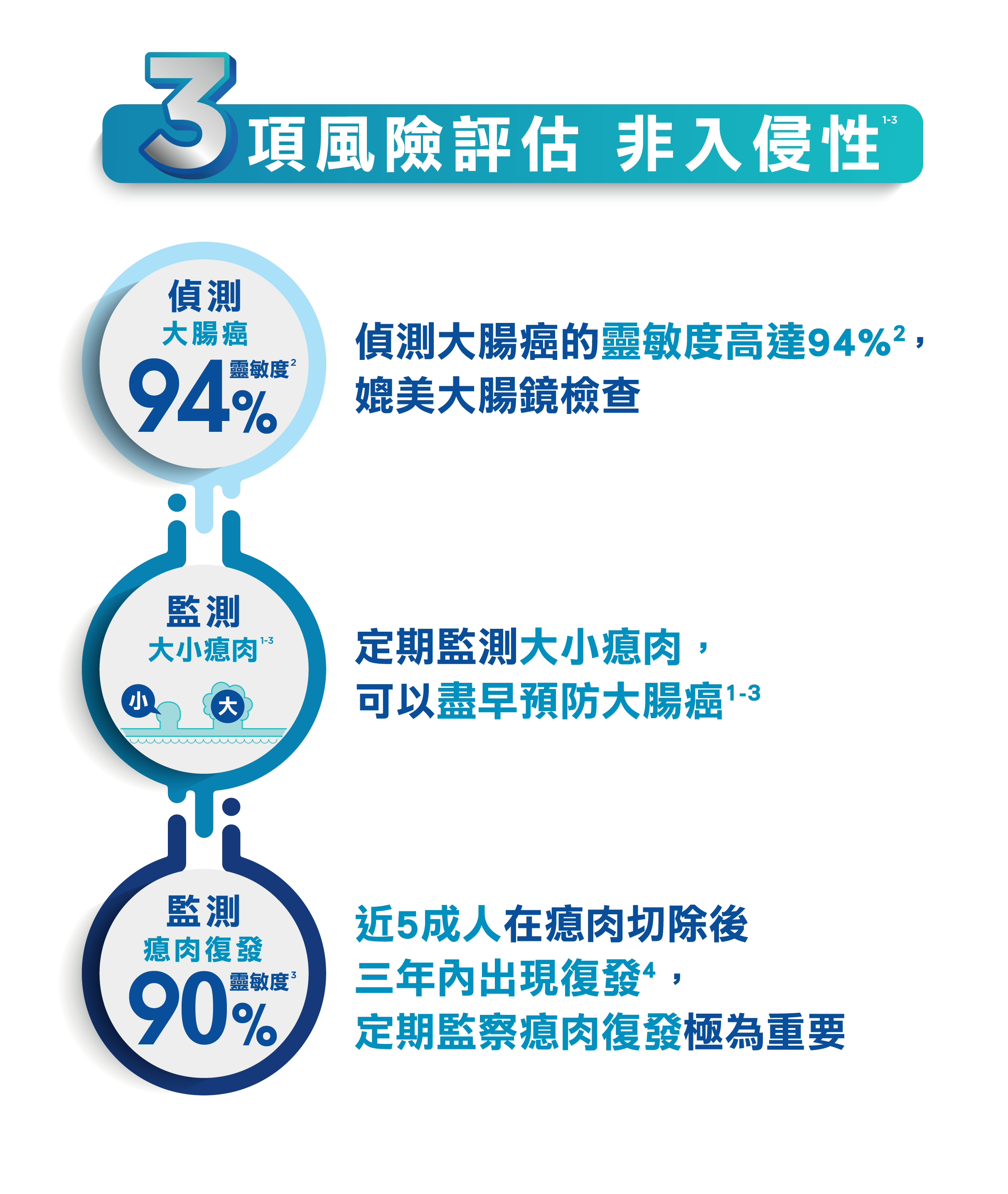
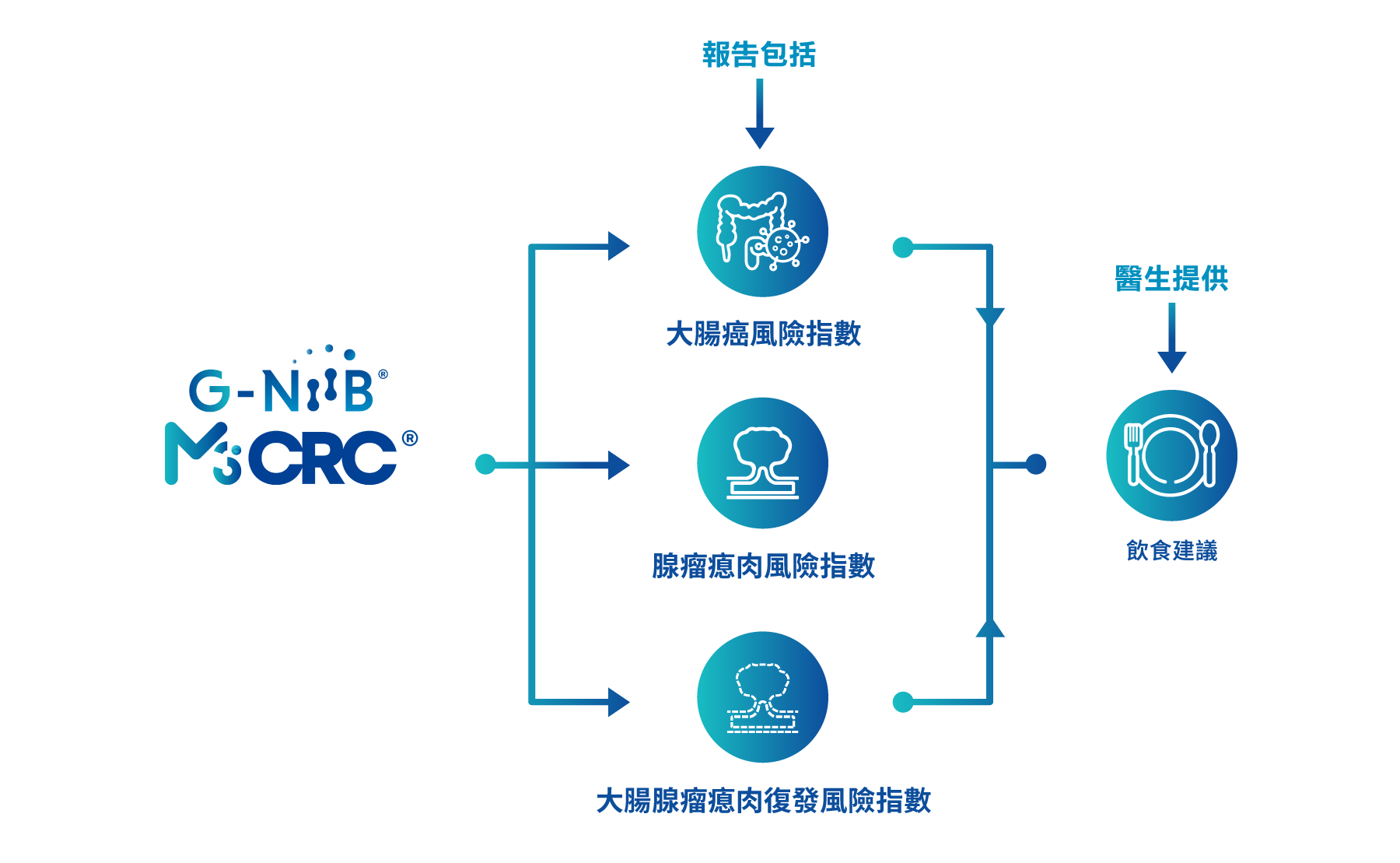
How does G-NiiB M3CRC predict the risk of colorectal cancer, adenoma and adenoma recurrence?
G-NiiB M3CRC measures the levels of M3 bad bacteria (patented discovery by the Faculty of Medicine of A Renowned University in Hong Kong) plus hemoglobin in the stool. Using our propriety algorithm, we generate 3 risk indices corresponding to risks of colorectal cancer, adenoma and adenoma recurrence. Higher risk indices reflect higher risks of having colorectal cancer, adenoma and adenoma recurrence.

Colorectal Adenoma Risk Index
Colorectal Cancer Risk Index

Colorectal Cancer Adenoma Recurrence Risk Index
The Advantages of G-NiiB M3CRC
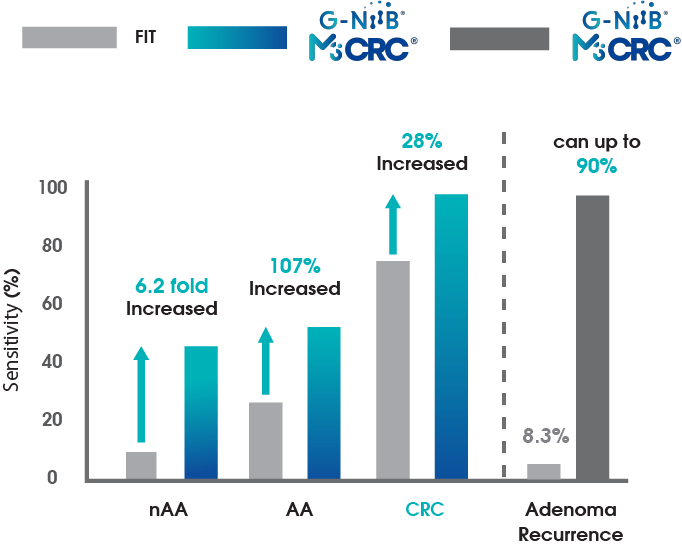
G-NiiB M3CRC is the World’s FIRST NON-INVASIVE Colorectal Cancer Risk Prediction Test that detects non-advanced adenoma and adenoma recurrence with High Sensitivity. The sensitivity of CRC detection is 94%, which is comparable to colonoscopy10 and the specificity is 85%. The sensitivity of adenoma detection is superior to the currently available non-invasive tests (especially for small polyps)1
Adenoma Recurrence
Can up to 90%3
*at 85% specificity
CRC: colorectal cancer
AA: advanced adenoma
nAA: non-advanced adenoma
A novel tool for monitoring gut microbial health
A persistently high score indicates a hostile microbial environment that is favorable for the development of CRC.
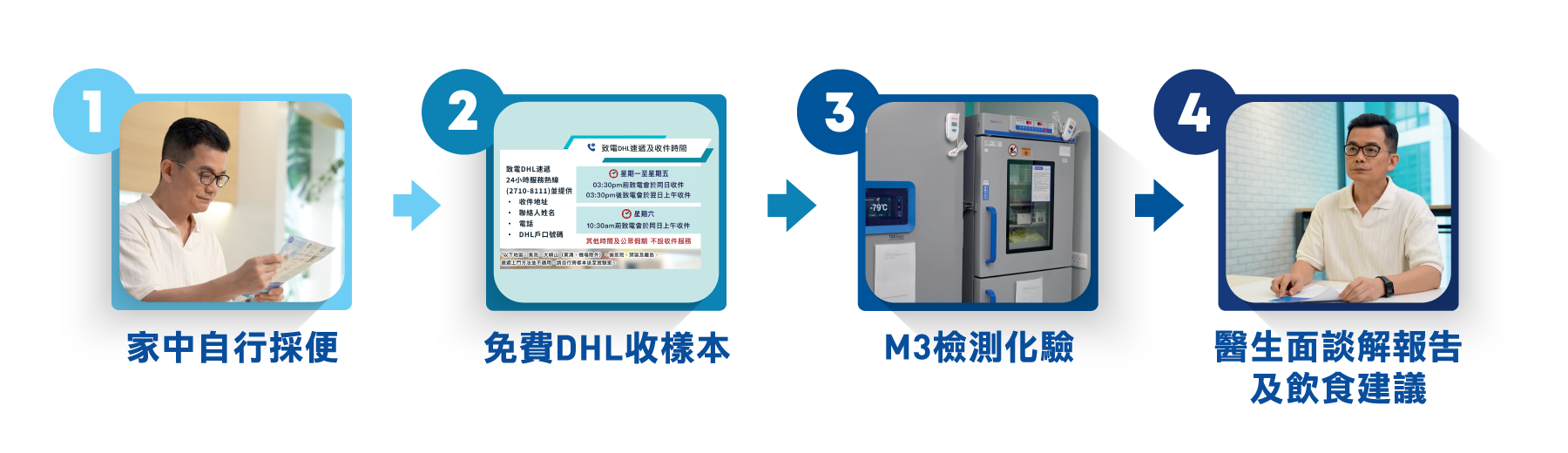
Flexible stool collection at home
Please follow this video guide to collect the stool sample.
To ensure the accuracy of the testing, please read the following notes carefully:
- Maintain regular diet within 2 weeks;
- Avoid antibiotics within 4 weeks;
- Avoid probiotics within 4 weeks;
- Do not collect the stool sample when it is watery due to diarrhoea and when there is bleeding from haemorrhoids and menstruation;
- Follow this Guide to collect the sample carefully. Return the sample within 24 hours.